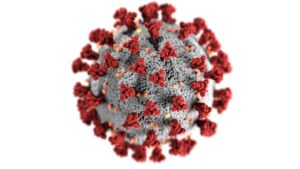
Yes, it comes from monkeys. That was your question, right? Now let’s get to what it is exactly!
Monkeypox is a very rare virus that can be passed from monkeys and other animals to humans. It’s also known as pox or smallpox. Most people who get monkeypox don’t have any symptoms, but when they do appear they are usually mild.
If you catch it early enough, you can treat it at home; however, if it gets out of control, it could lead to potentially serious complications. Luckily there are ways to prevent contracting the disease. Keep reading for more information about how to avoid getting infected with Monkey Pox and its treatment.
Monkey Pox: Details
The virus has never been reported in humans in the US, but it can pop up in places where people are in contact with infected animals, like African countries and tropical areas in South America. Monkeypox gets its name from the fact that it was first discovered in monkeys.
People get infected with the virus when they’re in contact with a monkey or other animals like rodents that carry the infection, according to the CDC. Humans can also get infected from breathing in the droplets from an infected person’s cough or sneezing.
How Do You Get the Monkey Pox Virus?
The disease that’s only found in certain areas of the world, like Africa and tropical areas of South America. You can get it from coming into direct contact with infected animals, like monkeys or rodents, or through the air when someone coughs or sneezes.
While it’s extremely rare to find monkeypox in the U.S., it can happen when people travel to areas where the virus is present and bring it back home with them. If you’re in a situation where you or others may come into contact with infected animals, you should take extra precautions. Wear gloves when handling them, and try to avoid being bitten or scratched. Cover all cuts, scratches, and open wounds with bandages, and make sure to keep them dry. Be sure to frequently wash your hands and thoroughly clean and disinfect all surfaces that may have come into contact with the virus as well. Are sounds familiar, doesn’t it?
Symptoms
Most people who get monkeypox don’t have any symptoms, but when they do appear they are usually mild. The average incubation period is 12-14 days. You can get a rash – bumps on your skin that form a red or blue spot – swollen lymph nodes (small glands in your body that fight infection) – pain and/or itching at the site of the rash. Other symptoms include fever headaches, nausea, muscle aches, diarrhea, and bleeding inside the stomach or intestines.
Treatment
If you think you’ve been infected with his virus, you should contact your doctor immediately. They can test your blood to see if it has been infected and you should stay away from others while you’re being tested.
Monkeypox can be treated. Your doctor will likely prescribe antibiotics if you’re diagnosed with the infection. You might also be given antiviral drugs to slow the progression of the infection.
Prevention
If you travel to areas that have a high risk of the virus, make sure you follow the recommendations mentioned above. Because it’s a rare infection, health officials don’t recommend vaccines, and they’re only available in certain countries.
Conclusion
Monkeypox is a very rare virus that can be passed from monkeys and other animals to humans. Most people who get monkeypox don’t have any symptoms, but when they do appear they are usually mild. Luckily there are ways to prevent contracting the disease. Some precautions are to wear gloves when handling animals and try to avoid being bitten or scratched by them and follow the cleaning recommendations mentioned in this article, but if you are afraid of catching the disease, the best suggestion is to not go to the high-risk areas.