![]()
2025 Update
Personal hypertension management has made its way into the mainstream. Mobile apps such as HealthHeart and Braun Healthy Heart have made them into the mainstream. These are mobile devices that come with sphygmomanometers (those blood pressure cuffs we see the doctors use when we visit them). They use the latest technology to monitor your blood pressure. Check them out at the App Store or Google Play.
Overview
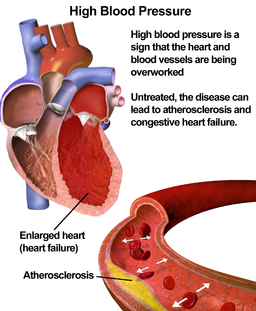
With no symptoms, high blood pressure (HBP) can sneak up on a person and escalate to any number of diseases that could result in death.
Without being tested for HBP, a patient might never know that HBP, also called hypertension, may be damaging his/her arteries, heart, and other organs.
Studies
A recent study from the American Heart Association found that keeping systolic blood pressure below 140 mm Hg reduces the risk of stroke for people aged 60 years and older. The study looked at the new systolic blood pressure target, which was 150 mmHg as recommended for older people who don’t have chronic kidney disease or diabetes, but determined that raising the target could put the population at a greater risk of stroke.
“We started this analysis very soon after [the JAMA paper] came out … because we were concerned about the recommendation’s potential effect on stroke prevention,” study author Ralph L. Sacco, MD, professor and chair of neurology at the University of Miami Miller School of Medicine, said in a statement.

The study looked at 1,750 people who were free of stroke, diabetes, and chronic kidney disease. Participants with a systolic blood pressure of 140 to 149 mmHg had an elevated stroke risk that was equal to participants with systolic blood pressure greater than 150 mmHg. The risk of increased stroke was most notable among Hispanics and blacks.
According to Dr Sacco, more aggressive treatment of blood pressure, especially among blacks and Hispanics, is even more critical. He added that the findings support the American Heart Association’s guidelines for treating blood pressure above 140 mmHg.
“The findings suggest one should not liberalize or change the treatment threshold for blood pressure in people older than 60 without chronic kidney disease or diabetes,” Dr. Sacco said. “For stroke prevention, maintaining a blood pressure target of 140 mmHg is important.”
Symptoms
 HBP does not have any symptoms except in the extreme case of a hypertensive crisis. However, there are many misconceptions. For example, there is no actual evidence that HBP causes headaches.
HBP does not have any symptoms except in the extreme case of a hypertensive crisis. However, there are many misconceptions. For example, there is no actual evidence that HBP causes headaches.
In addition, nervousness, sweating, difficulty sleeping, and facial flushing are not signs of HBP either. Other symptoms that are sometimes thought to be signs of HBP but have no scientific link include nosebleeds, blood spots in the eyes, and dizziness.
Don’t wait for symptoms before taking care to prevent or get diagnosed with high blood pressure. Left untreated, hypertension can cause heart attacks, heart disease, heart failure, stroke, vision loss, memory loss, and kidney disease, among other health consequences.
 Diagnosing is quick and painless—healthcare professionals use a blood pressure monitor, and a cuff is placed on the upper arm and inflated. The cuff momentarily stops blood flow, then slowly releases. Optimal blood pressure is less than 120/80 mm Hg.
Diagnosing is quick and painless—healthcare professionals use a blood pressure monitor, and a cuff is placed on the upper arm and inflated. The cuff momentarily stops blood flow, then slowly releases. Optimal blood pressure is less than 120/80 mm Hg.
Some patients are at a higher risk of developing HBP. Certain groups have a higher risk—for instance, African Americans have a higher risk than other racial groups, and after age 65, women are more likely to have HBP than men.
Risk factors for developing hypertension include family history, advanced age, lack of physical activity, poor diet and a diet high in salt, being overweight or obese, heavy and regular use of alcohol, stress, smoking, and sleep apnea.
However, some of the factors can be controlled. While there isn’t much that can be done about family history, race, or age, the other risk factors can be treated.
 If you are diagnosed with HBP, medication is not the only method that can reduce high blood pressure. Losing weight (even as little as 10 pounds); exercising regularly (at least 30 minutes multiple days a week); eating a diet rich in whole grains, fruits, vegetables, and low-fat dairy products; reducing alcohol intake; quitting smoking; and either limiting or better coping with stress are all factors that are under your control. So why wait? With a bit of willpower, you can make these changes!
If you are diagnosed with HBP, medication is not the only method that can reduce high blood pressure. Losing weight (even as little as 10 pounds); exercising regularly (at least 30 minutes multiple days a week); eating a diet rich in whole grains, fruits, vegetables, and low-fat dairy products; reducing alcohol intake; quitting smoking; and either limiting or better coping with stress are all factors that are under your control. So why wait? With a bit of willpower, you can make these changes!