What is RSV?
Respiratory syncytial (sin-SISH-uhl) virus, or RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious, especially for infants and older adults. RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs) in children younger than 1 year of age in the United States.
Respiratory Syncytial Virus (RSV) is an extremely common but contagious illness that infects the lungs and breathing passages and is the most common cause of bronchiolitis. It can spread through the air, contact with secretions (such as saliva, mucus, and tears), or contact with contaminated objects and surfaces.
While many cases of RSV are mild and cause no more than a few days of coughing and a runny nose, some cases can be more severe and lead to serious complications, especially for children. It is important to understand the symptoms, diagnosis, and treatment of RSV to recognize the virus and get appropriate medical care.
How Serious is RSV?

If you are exposed to RSV as an adult, you might have a bout of coughing and a runny nose and feel like you have the flu.
Babies and young children could become ill to the point of hospitalization.
RSV causes more deaths in children under one-year-old than any other type of infection.
Babies and young children are at risk for serious health problems and even death if they get infected. According to a recent study, one in every fifty children die from this disease in low-income and middle-income countries. At this age, the immune system is still developing, and babies are at greater risk for serious complications from the infection.
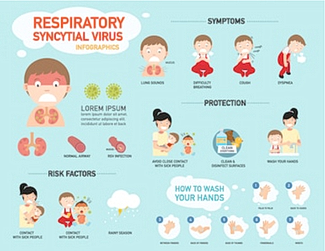
Symptoms
Symptoms usually appear about four to six days after acquiring the infection. If you are an adult you most likely will have just mild cold-like symptoms.
These symptoms may include:
- A cough that may or may not produce sputum (phlegm)
- Runny nose
- Asthma or wheezing
- Shortness of breath
- Hard time sleeping
- Fever
Diagnosis
If you have these symptoms or others, your doctor will likely ask about your medical history, but he/she will be unlikely to order any tests because there is no specific diagnosis for RSV.
To rule out other conditions and determine the best course of treatment, your physician may order tests such as a blood test, chest X-ray, or sputum (phlegm) cultures. These tests are usually done only if you have a child that is younger than two months old or if you have a complicated or severe case of RSV.
Complications
In severe cases, there may be a few complications that can occur.
- Breathing Problems – RSV can cause wheezing, a whistling sound in the lungs (stridor), rapid breathing, and slow or irregular heart rate. In severe cases of RSV, these breathing problems can require treatment in the hospital, including a breathing tube (intubation).
- Pneumonia – If you have significant difficulty breathing and have a high fever, you may have a bacterial infection in the lungs, which can develop as a complication of RSV. Bacterial pneumonia can be serious and needs to be treated with antibiotics.
- Swallowing Problems – Since the respiratory system and the digestive system are close together, RSV can also affect the esophagus, the tube that connects the throat to the stomach. If a baby or young child with RSV develops significant sputum in their throat, they may have trouble swallowing and aspiration (taking in) their saliva and mucus. Esophagitis can occur in both breastfeeding and non-breastfeeding infants. If it is recognized early and treated, most cases resolve without complication.
Treatment of RSV

There is no specific treatment. Instead, doctors support and treat the symptoms as they arise. If you have severe or life-threatening issues, you may need to be hospitalized to get more focused care.
For milder symptoms, take the following steps to support your body and allow the virus to pass without complications: – Rest and rest as needed. If you are not breastfeeding, it is best to rest for a few days.
If you are breastfeeding, you may still want to rest as needed. – Drink plenty of fluids. You can take in fluids by drinking water, juice, or sports drinks. You may also want to take in electrolytes through gels or packs. Avoid drinking carbonated beverages as these can lead to increased vomiting. – Take a pain reliever as needed for any coughing or pain. – Ask for help with childcare and housekeeping.
Prevention

There is no way to prevent RSV completely. However, taking steps to prevent the transmission of the virus can help reduce the risk of getting infected. The list below has been stated previously in other articles on respiratory diseases, but it never hurts to reiterate!
- Wash hands regularly with soap and warm water for at least 20 seconds.
- Avoid touching your face and then touching your baby. This includes coughing and sneezing into your elbow, not your hands.
- Avoid close contact with infants who have RSV.
- Avoid crowds, especially if you are breastfeeding.
- Avoid places with poor air quality.
RSV in Infants and Young Children
For infants and young children, RSV can cause serious illness and even death. Babies under two months of age are at the highest risk for complications from RSV, including death.
The following signs may indicate that your child has RSV and should be checked by a doctor:
- Increased breathing rate or difficulty breathing
- Coughing that produces thick or colored sputum
- Poor feeding (e.g., appearing lethargic or sleepy, not feeding well, looking irritated or stressed when feeding)
- Blue or purple coloring of hands and feet
- Poor weight gain. If your child has any of these symptoms, you should contact your doctor right away to discuss their illness and get medical advice
When to Seek Medical Care
If you have any symptoms of RSV, particularly if you are breastfeeding and have an infant, it is important to contact your doctor. If your child has severe symptoms, you should seek medical care. If your child is less than two months old and has any of the following symptoms, they should be seen by a doctor: – Breathing difficulty – High fever – Poor weight gain.
Outlook
Most people with RSV recover without any complications. It is important to rest and drink plenty of fluids to reduce the severity and duration of symptoms.
In some cases, people with RSV can develop pneumonia. If someone develops pneumonia, they may need antibiotics. If the infection spreads to the bloodstream, some people will need to be hospitalized and may need antibiotics to treat it.
If your child has RSV, it is best to rest and take care of yourself as well. Taking good care of your health can help you take better care of your child.
If you were born between 1947 and 1957, you may have been exposed to a different type of RSV as a child. The infection was less common and often more severe, with a higher risk of complications and death. While you will have immunity to the type of RSV that is more common today, you may be at risk for a severe infection if exposed to the older type.