Overview
Nutritionists, health professionals, and virtually all health experts have long promoted the nutritional benefits of eating fish. Both vegetarians and omnivores enjoy fish as a main source of protein. It’s not only high in protein, but fish is also the best source of heart-healthy omega-3 fatty acids, selenium, B-12, and Vitamin D that fights inflammation.
Wild or Not?
The recommendation is to only buy the wild variety, as many versions of fish that are farmed contain very low amounts of nutritional benefits such as omega-3s when compared to their wild counterparts. Let’s delve a bit more into this.
Farmed Fish
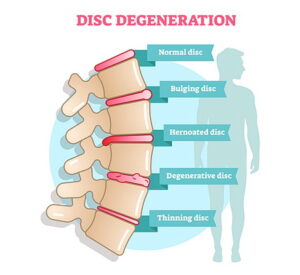
Farmed fish are also fed unnatural diets that contain animal products, soy, and dye. The essential omega-3 nutrient found in wild fish plays an important role in our bodies. Research shows that omega-3 fatty acids decrease inflammation in the body such as joint swelling and pain. It’s also been shown to moderately improve ADHD and anxiety symptoms.
Wild Fish
Unfortunately, wild fish contains varying amounts of mercury which is harmful in large doses. It can cause adverse neurodevelopmental, cardiovascular, and immunological health effects. Pregnant women should avoid eating fish that are highest in mercury at 500 parts per billion and over, while other women and men should avoid eating fish that contains 1,000 parts per billion of mercury.
With that said, wild salmon is still considered one of the healthiest salmons to eat and provides the following:
-
-
- Omega-3 fatty acids
- Protein
- Potassium
- May reduce the risk of heart disease
- May help in weight reduction
-
So What Fish Should We Eat? Take Your Pick!

-
-
- Light canned tuna is a cheap and quick source of protein. It contains only 118 parts per billion of mercury and is very high in omega-3s.
- Wild Atlantic cod only contains 70 parts per billion of mercury and is shown to help lose visceral fat and improve blood pressure when eaten once to three times a week.
- Almost all shellfish including mussels, shrimp, lobster, and oysters contain very low levels of mercury and are very high in B-12 and omega-3s as well as iron.
- Squid and calamari contain very low levels of mercury and very high levels of omega-3.
- Wild trout has very high levels of omega-3s and is a lean protein, but should be avoided because of its moderate polychlorinated biphenyl contamination.
- Wild Atlantic mackerel, wild halibut, Atlantic pollock, canned sardines, and European anchovies make the best choice for fish you can eat daily. All of these fish contain very low mercury levels and very high omega-3 levels.
- Fish such as shark, swordfish, king mackerel, tilefish, northern pike, and albacore tuna should be avoided as they contain high levels of mercury. As a rule of thumb to remember, usually the bigger the fish the more mercury it contains.
- Every variety of wild-caught salmon from Alaskan salmon to Southeast Alaskan chum, sockeye, coho, pink, and chinook salmon, as well as Kodiak coho and chum salmon, are considered the lowest risk fish for consumption because of their low levels of mercury and other contaminants.
- As mentioned, all wild-caught salmon contain very high levels of omega-3s. Recent studies have found that this wonder fish also contains small bioactive protein molecules that may provide special support for joint cartilage, insulin effectiveness, and control of inflammation in the digestive tract. The selenium found in wild-caught salmon decreases the risk of joint inflammation and also helps prevent colorectal, breast, and prostate cancers, and is also important in heart health.
-
Summary
Eating fish of any type will be a benefit to your health, but be careful with the wild kinds as they may contain a larger amount of mercury which can be harmful to your body.
Of all the types listed here, we believe that salmon would be the most beneficial. If you do want to go for the wild type, such as wild salmon, speak to a medical professional or your doctor first to confirm that it will not be overly harmful to you.