
Immunization Overview
The human immune system is a complicated network of cells and proteins that defends the body against foreign invaders, including viruses and bacteria. In this post, we look at how the immune system responds to the COVID-19 virus.
Since this disease is relatively new, there is a lot that we still need to learn about and several questions remain regarding the immunity to the virus, both following the infection and immunization and so the research continues. One factor that is accepted throughout the world is that those who have strong immune systems fare better than those that are immune-compromised and/or are part of the elderly community.
It is important to note that natural immunity refers to how your natural immune system responds following the infection, whereas vaccine-induced immunity is the process by which a COVID injection stimulates your immune system to produce more antibodies – enough to prepare your body to resist the virus should you get infected.
Here, we look at how the immune system works against COVID-19 and how the immune system responds following the infection and vaccination.
How Long Does COVID-19 Immunity Last Following the Infection?

This is a very good question and there has not been a definitive answer; however, researchers believe it could be anywhere from between three to eight months.
The claim is based on several pieces of research performed to analyze the antibodies in individuals who were infected by the virus. However, the results of these studies vary significantly as the life of antibodies targeting the spike of SARS-CoV-2 varies from individual to individual. Moreover, other factors besides antibodies, such as T and B cell memory, affect the natural immunity against COVID-19.
As of now, they suggest booster shots after six months of being vaccinated. Since COVID-19 is a relatively new disease, researchers worldwide are continuing their quest to find out how long the body defends itself against the disease.
It cannot be definitively concluded how COVID-19 immunity lasts following the infection, but let’s look at each of the components that can affect the natural immunity against COVID-19.
Antibodies – How Long Do They Stay in the Body?
As mentioned, the search and destroy army of antibodies can last for several months in patients infected with COVID-19. However, the number of antibodies tends to decrease over time. One of the studies that included 5882 people who had recovered from this pathogen concluded that the antibodies were still present in the blood five to seven months following the infection. The results hold true for patients with both mild and severe illnesses. Moreover, there was evidence that people with severe COVID-19 illness ended up with more antibodies compared to those with a mild infection.
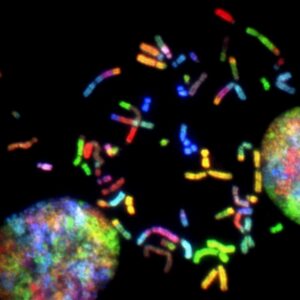
T and B Cell Response – An Integral Part of Immunity
While the antibodies developed as a response to the infection and play an important role in protecting against future infection, T and B cells also have a central role in fighting off infections. The T and B cells are the only cells in the immune system that can recognize and respond specifically to a virus as they are memory cells. These highly specialized memory cells can stay in your system for years and even decades and continue to trigger the immune system response when your body interacts with the same virus.
One study conducted by science.org was to find out the presence of T and B cells in individuals who have had COVID-19. T and B cells are cells that remember the previous diseases and act on them if they return. The results concluded that even when the antibodies fell, memory T and B cells were present for as long as up to eight months following the infection. However, the only limitation of this study and other similar studies is that we have limited evidence since COVID-19 is a relatively new disease. Given this lack of definitive conclusions, we cannot, at this time, be sure about how long the T and B memory cells stay in the body once exposed to SARS-CoV-2.
Vaccine-Induced Immunity – Immunity Developed Following the COVID-19 Immunization
And while the researchers assess the natural immunity against COVID-19, it is critical to assess the vaccine-induced immunity to determine the effectiveness of COVID-19 immunization and the need for a booster for the COVID-19 vaccine.
Several studies worldwide are being conducted to determine how long immunity lasts following COVID-19 immunization. A relatively new study found a surprisingly higher number of B cells (memory cells) among individuals immunized using Pfizer’s mRNA vaccine. The participants received their second dose of the mRNA vaccine at least 12 weeks before assessing their immunity. The participants included people who were not previously infected by COVID-19.
So far, the research conducted to determine vaccine-induced immunity suggests that the mRNA vaccine is likely to generate a durable and lasting immune system response; however, further evidence is required to confirm the claim.
How Vaccine-Induced Immunity Varies Between the First and the Second Doses?

Given how the immune system responds after one dose of the vaccine as opposed to two is difficult to assess. However, multiple studies have investigated that the antibody level in the blood varies at different stages between the two doses.
A study involving over 50,000 participants concluded that 96.4% of the participants had positive antibodies one month following their first dose of Pfizer and AstraZeneca vaccines. Additionally, 99.1% of the participants had positive antibodies seven and 14 days following their second dose of the vaccine. Furthermore, the antibody levels changed slightly up to two weeks following the second dose. Other similar studies were also conducted, and the results showed that the vaccine-induced immunity varies between the first and the second doses of the mRNA vaccine.
Comparing Natural Immunity with Vaccine-Induced Immunity
The exposure to SARS-CoV-2 and resulting infection and COVID-19 immunization (with mRNA vaccine) have shown an immune system response generated by memory T and B cells and the creation of antibodies. However, there is a stark difference in how the immune system responds to natural infection and to the vaccine.
The immune system’s response to the COVID-19 vaccine is fairly homogeneous, and data suggest that the mRNA vaccine results in T and B cell reactivity. However, how long does immunity last among individuals following infection, and how strong of immune system response is generated following the infection is still not definitive?
Will COVID-19 Vaccine Boosters Be a Necessity?
Given how the antibodies and the T and B memory cells behave following immunization, a key question that still remains is whether COVID-19 vaccine boosters are a necessity? The answer is still not clear; however, Albert Bourla, the CEO of Pfizer, explains the need for a booster vaccine within 12 months following the second dose.
The reasons include weaker immune system response over time, especially among older adults. Moreover, the SARS-CoV-2 is mutating, and new variants are emerging, which could be a possible threat to individuals, especially the ones with weakened immunity; hence, on September 22, 2021, the FDA amended their emergency vaccine procedure to include booster shots for specific criteria of people – those age 65 and over, are immune-compromised and/or work in healthcare facilities.
Summary
In general, there are three ways we can have our immune system fight off the COVID virus, through natural immunity, the vaccine’s creation of antibodies, and T and B memory cells that will recognize and attack the virus if it comes back. But research is still going on to determine how long the vaccine and antibodies remain in the body, but after the first, second, and third doses.
So far, it appears that after the first and second doses of Pfizer or Modena, the antibodies can last for good six-twelve months, but diminish as the months proceed. Booster shots are recommended for individuals with weaker immune systems after around six months.


 The problem is that Individuals who suffer from blood cancer, such as leukemia, lymphoma, or multiple myeloma may find that the COVID-19 vaccine leads to a lowered immune response. However, this is the norm for all vaccines when it comes to these individuals. However, immunocompromised individuals are strongly recommended to get the vaccine as it still provides them with some sort of protection.
The problem is that Individuals who suffer from blood cancer, such as leukemia, lymphoma, or multiple myeloma may find that the COVID-19 vaccine leads to a lowered immune response. However, this is the norm for all vaccines when it comes to these individuals. However, immunocompromised individuals are strongly recommended to get the vaccine as it still provides them with some sort of protection.







 According to an independent analysis published in November 2020, Pfizer-BioNTech announced 95% effectiveness of their BNT162b2 vaccine.
According to an independent analysis published in November 2020, Pfizer-BioNTech announced 95% effectiveness of their BNT162b2 vaccine. 


