September 2023 – Covid Vaccine UPDATE
Pharmaceutical company Moderna has said that its new vaccine booster works against this new virus variant, and as of September 2023, you can get the booster at your local pharmacy.

Here Comes BA.2.86, Maybe
Most of us believe that the Sars-CoV-2 Coronavirus (COVID-19) is behind us and that we can go about our regular daily routines without having to worry about catching it again. Well, maybe that’s true. Then again, maybe not.
A new variant called Pirola, technically labeled BA.2.86, is starting to show its ugly face, and according to some sources, it is spreading rapidly around the United States and the world.
So What Exactly is BA.2.86?

The BA.2.86 variant was first detected in Denmark and Israel in late August 2023 and has since been found in several other countries, including the United States.
According to researchers, this particular virus is a subvariant of Omicron, the most dominant variant of SARS-CoV-2. BA.2.86 is more transmissible than the other Omicron subvariants.
How Transferrable is this Variant?
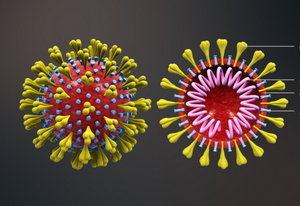
Scientists say that it may be more resistant to the current vaccines and antibody treatments. This is because BA.2.86 has a number of mutations in its spike protein, which is the part that the virus uses to attach to your cells. However,
How severe is BA.2.86?
It is still too early to say whether this variant is more severe than the others. More studies are needed to determine its severity. However, some early studies have suggested that it may be more resistant to current vaccines and antibody treatments.
How can I protect myself from BA.2.86?
Maintain the standard methods of keeping clean, which include washing your hands frequently, carrying an antibacterial cleanser, avoiding large crowds, and avoiding close contact with people who are sick, to name a few.
Additionally, get vaccinated and boosted. Vaccines are still very effective at preventing serious illnesses and hospitalization from COVID-19, even against the new variants.
Although most people have stopped using masks, if you feel more comfortable wearing one when outside, by all means, do, especially when in crowded areas.
Who are Most Affected?

As with all the Covid-19 viruses or, more generally speaking, with any viruses, if you are elderly, have health issues, or have a compromised immune system, you should be vigilant and take all the recommended precautions.
Additionally, when any new disease is circulating in your area, you should also speak to your medical provider for any additional precautions you may need to take.
Conclusion
Staying attentive to COVID-19 is nothing new. Even though a new variant has materialized, that doesn’t mean you have to run to your bed and hide. Research is determining that this virus may be more transmissible than the previous subvariants and possibly more resistant to the current vaccines, but as research continues on the BA.2.86 virant, it may turn out that it is not as contagious as the other. It is just a wait-and-see game.
The general recommendations are to just stay vigilant and maintain the COVID rules of keeping clean and safe, especially if you are in the high-risk health category.