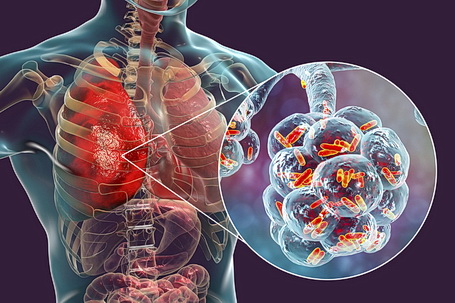
Pneumonia is an infection of one or both lungs that leads to the production of pus. The infection causes the delicate lung tissue to become inflamed, and filled with fluid and creates a hospitable environment for bacteria.
Acquiring bacteria and viruses in the air we breathe is the most common cause of pneumonia. Your body will typically defend your lungs against these germs but sometimes, even if you are in good health, your immune system might not be able to fully neutralize the infection. With that said, under normal conditions and if you are in good health, you should fully recover within a week or two.
But, pneumonia can also be a life-threatening condition that requires treatment in a hospital, especially for the elderly and/or immune-deficient individuals. These more serious cases are known as severe and can lead to long-term consequences such as chronic lung disease or even death.
Different types of pneumonia can be broadly categorized as community-acquired or hospital-acquired pneumonia. Learn more about this condition in this article.
What is the Difference Between Community-Acquired Pneumonia (CAP) and Hospital-Acquired Pneumonia?
Community-acquired pneumonia (CAP) is caused by bacteria present in the environment outside of a hospital. CAP occurs when bacteria enter the lungs through the airway and multiply there. This can happen when you have a cold, or another virus.
Hospital-acquired pneumonia (HAP) is a type of pneumonia that develops in a patient who has been admitted to the hospital, usually due to an infection that the patient already has, such as a urinary tract infection, blood infection, or lung infection.
It is a type of healthcare-associated infection (HAI). This means the person contracted it while being treated for another condition in a healthcare setting, such as a hospital.
It is important to note that not all pneumonia acquired in a hospital setting is also healthcare-associated pneumonia. HAP can be life-threatening for patients and can occur after surgery, as a complication of other infections, or as the result of the use of breathing machines. It is therefore important for healthcare providers to follow infection prevention and control practices to reduce the risk of contracting HAP and spreading it to other patients.
Pathophysiology of Pneumonia

An infection in the lungs can cause inflammation and fluid buildup in the air sacs (alveoli) of the lungs.
The infection can be caused by a virus, bacteria, or other microorganisms. It can also be caused by inhaling irritants such as dust or fumes.
Bacterial pneumonia is when bacteria infect the lungs and cause an infection. Viral pneumonia is when a virus infects the lungs and causes an infection.
Diagnosis of Pneumonia
Pneumonia can be diagnosed based on symptoms, physical exams, and lab tests. Healthcare providers may order a chest X-ray to confirm if there is an infection in the lungs and if there is pneumonia. Blood tests can also be done to check for bacteria and other microorganisms. Additionally, a cat scan may be used to further determine the infection and possibly the cause.
Severity of Pneumonia
The severity is determined by how quickly the condition progresses. The two main factors that determine how quickly a patient might progress with pneumonia are the person’s overall health before getting the infection and if there are any other health conditions present.
People who are generally in good health have a lower chance of progressing to a severe level compared to people who have preexisting medical conditions. Patients with mild pneumonia may not have any symptoms other than a cough that may be so mild that it can be mistaken for a chronic cough.
Mild
Pneumonia is considered mild when patients have a mild cough (that can be mistaken for a chronic cough), an unexplained fever, and/or shortness of breath, as well as other cold-like symptoms.
Its technical name is atypical pneumonia, but it is more commonly known as walking pneumonia since seeking a medical professional is not required, but recommended and the patient can go on with his/her daily routine although feeling like he/she has a bad cold.
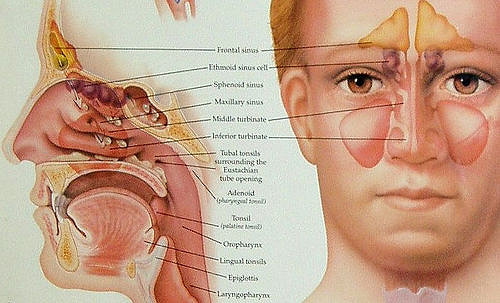
Walking pneumonia is most commonly caused by a bacteria known as Streptococcus pneumoniae, which is typically found in the upper respiratory tract. Approximately 900,000 Americans are found to be infected with this bacteria each year.
Severe
Pneumonia is considered severe when the patient’s symptoms are exactly that – severe, meaning that your cough, fever, headaches, shortness of breath, etc. are enough to make you feel so uncomfortable that you want to seek medical attention. (This is not to say that you shouldn’t seek medical attention or advice if you have a mild case). Hospitalization is required for the treatment of severe pneumonia because symptoms such as breathlessness, chest pain, and fatigue become more severe.
Treatment for Pneumonia
Pneumonia is treated in several ways, depending on the patient’s overall health and the severity of the infection. Treatment for mild bacterial pneumonia is usually limited to antibiotics and plenty of rest.
For severe cases, patients are placed on mechanical ventilation if their breathing is too shallow or fast or their oxygen level is too low. If the patient is not on a ventilator, they may receive antibiotics intravenously to kill the bacteria causing the infection. Patients who are on mechanical ventilation are given antibiotics through a port placed in their veins as well as supplemental oxygen.
Prevention of Pneumonia
Vaccination is recommended for those who are at a high risk of getting the disease, such as people over 65. Other groups that can benefit from vaccinations include healthcare workers, people traveling to countries where pneumonia is common (such as developing nations), and people who have a weakened immune system.
Smoking tobacco is the leading risk factor for pneumonia as it damages the lungs, compromising their immune function and ability to fight infections.
Stress, particularly chronic stress, can also weaken the immune system and increase susceptibility to pneumonia.
There are also steps you can take to reduce the risk of pneumonia, including getting plenty of sleep and avoiding large crowds during flu season.
Conclusion
Pneumonia is an infection of the lungs that causes inflammation and fluid buildup in the air sacs (alveoli) of the lungs. It can be caused by a variety of microorganisms, including viruses and bacteria.
Symptoms of pneumonia include fever, cough, shortness of breath, and difficulty breathing, but it can be treated with antibiotics, rest, and fluids.
It is important to see a doctor if you think you may have pneumonia, as it can be fatal if left untreated for some people.
There are two types of pneumonia: community-acquired pneumonia and hospital-acquired pneumonia. Community-acquired pneumonia occurs when bacteria enter the lungs through the airway, either as a result of a viral infection or from exposure to irritants in the air.
Hospital-acquired pneumonia is an infection that results from an infection that the patient already has, such as a urinary tract infection, blood infection, or lung infection. It is important to note that not all pneumonia acquired in a hospital setting is also healthcare-associated.
If you do come down with any of these symptoms mentioned and these symptoms are precise beyond the normal course of time where they should have subsided, or if you are immune deficient, elderly, or have other high-risk issues, you should seek a medical professional ASAP!




 Generally, the procedure is performed as an outpatient at a hospital. An anesthesiologist is present to facilitate the process. Prior to undergoing surgery, patients must be examined i.e. their medical history must be studied and lab tests should be performed as well.
Generally, the procedure is performed as an outpatient at a hospital. An anesthesiologist is present to facilitate the process. Prior to undergoing surgery, patients must be examined i.e. their medical history must be studied and lab tests should be performed as well.








 If you are in the vicinity of a person with asthma, don’t light up your cigarette without asking. Smoking makes it difficult for an asthma patient to breathe and it may even trigger an
If you are in the vicinity of a person with asthma, don’t light up your cigarette without asking. Smoking makes it difficult for an asthma patient to breathe and it may even trigger an 