At a Glance
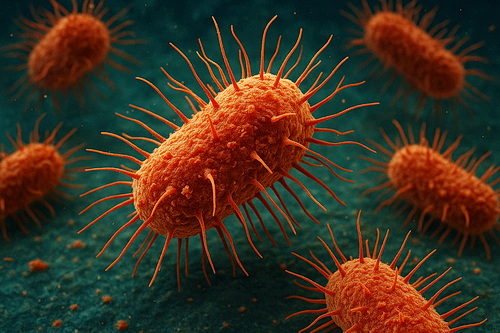
“Nightmare bacteria” is a nickname for certain germs that are extremely hard to treat because they resist almost all antibiotics, even the strongest ones doctors normally use as a last resort. These bacteria spread mainly in hospitals and nursing homes, can cause severe infections such as pneumonia and bloodstream infections, and are dangerous because they leave doctors with very few treatment options. Prevention through good hand hygiene, careful use of antibiotics, and strict hospital cleaning practices is the best way to stop them from spreading.
Infection rates have increased 70% from 2019 – 2023. Let’s take a closer look at what this is all about.
What Are “Nightmare Bacteria”?
The phrase “nightmare bacteria” is used by the Centers for Disease Control and Prevention (CDC) to describe superbugs that are nearly impossible to treat with today’s antibiotics. The most common example is a bacterial group called carbapenem-resistant Enterobacterales (CRE).
These bacteria are part of the same family as E. coli and Klebsiella, which normally live in our guts without causing harm, but when they become resistant and spread in the wrong places, they can cause very serious infections.
Why Are They Called “Nightmare?”
-
- Few medicines work: Even “last-resort” antibiotics often fail.
- They spread resistance: They can pass along their “superpower” to other bacteria, making those harder to treat, too.
- They are deadly: Up to half the people who get bloodstream infections from these germs may die.
- They thrive in hospitals: They show up most often in people who are already very sick, especially in intensive care units or nursing homes.
- Few medicines work: Even “last-resort” antibiotics often fail.
Where Are They Found?
Nightmare bacteria mostly spread in healthcare settings like hospitals, rehab centers, and nursing homes. They are more likely to infect people who:
-
- Use medical devices like catheters or ventilators
- Have weakened immune systems
- Have been on antibiotics for a long time
|
What Kinds of Infections Do They Cause?
- Use medical devices like catheters or ventilators
These bacteria can cause:
-
- Blood infections (sepsis)
- Pneumonia
- Urinary tract infections (UTIs)
- Infections after surgeryThe problem is not just that they infect people, but that regular treatments do not work well, leaving doctors with only older or more toxic drugs.
- Blood infections (sepsis)
Can They Spread to Healthy People?
Healthy people in the community are at very low risk. Most cases happen in hospitals or nursing homes. But because the bacteria can live in the gut without making someone sick right away, patients can unknowingly carry them and pass them along.
How Do Doctors Treat Them?
Doctors have to rely on a few older, stronger antibiotics that come with more side effects. Sometimes, they even use combinations of drugs to try to fight the infection. Unfortunately, even with these treatments, many patients do not survive serious infections.
How Do We Stop the Spread?
The best way to fight nightmare bacteria is to prevent them from spreading in the first place.
-
- Hospitals and nursing homes: Careful handwashing, wearing gloves and gowns, and strict cleaning routines.
- Antibiotic use: Doctors must be cautious and avoid giving antibiotics unless they are really needed.
- Patient awareness: Families and patients should not be afraid to remind staff to wash their hands.
Frequently Asked Questions (FAQs)
- Hospitals and nursing homes: Careful handwashing, wearing gloves and gowns, and strict cleaning routines.
Should I worry about getting nightmare bacteria at home?
Not really. These germs are mainly a hospital problem.
Can kids or healthy adults get infected?
It is extremely rare. Infections mostly happen in people who are already very sick.
Is there a vaccine?
No, not yet. Prevention is through hygiene and careful use of antibiotics.
What can I do if a family member is in the hospital?
A: Make sure staff are washing their hands and following infection control rules. This makes a big difference.
The Technical Part
The term “nightmare bacteria” is mainly used to describe Carbapenem-Resistant Enterobacterales (CRE), especially the carbapenemase-producing ones (CP-CRE).
What Are You Talking About?
-
- CRE = bacteria from the Enterobacterales family (like E. coli or Klebsiella) that resist carbapenem antibiotics.
- CP-CRE = the most dangerous kind of CRE, because they actually produce enzymes (carbapenemases) that break down and destroy the antibiotic itself.
- The CDC called them “nightmare bacteria” because:
- They are resistant to nearly all antibiotics
- They can spread their resistance to other bacteria
- Infections can be deadly (mortality rates as high as 50%)
- CRE = bacteria from the Enterobacterales family (like E. coli or Klebsiella) that resist carbapenem antibiotics.
So when health officials or the media say “nightmare bacteria,” they are almost always talking about carbapenemase-producing CRE (CP-CRE).
Bottom Line
“Nightmare bacteria” are a serious health threat because they resist almost every antibiotic we have. They mostly affect people in hospitals and nursing homes, and once they take hold, they are very difficult to treat. Prevention, smart antibiotic use, and strict hospital hygiene are the best tools we have to stop them.
